Brai3n Research

Brain research center for advanced international, innovative & interdisciplinary neuromodulation is an academic translational research centre
BRAI3N research analyses the outcomes of patients, primarily for novel treatments developed by its partner universities, but also for industry partners, who are interested in evaluating whether a novel treatment results in a substantial benefit for the patient. Brai3n research is especially interested in external validation, and more specifically ecological validation of novel neuromodulation treatments.
What is the difference between Brai3n research and Brai3n clinic? Only when a treatment has shown a significant effect, are those novel treatments implemented in brai3n clinic. Brai3n clinic can be seen as an early adopter of new neuromodulation treatments. Brai3n research will make sure that these novel treatments are worthwhile clinically.
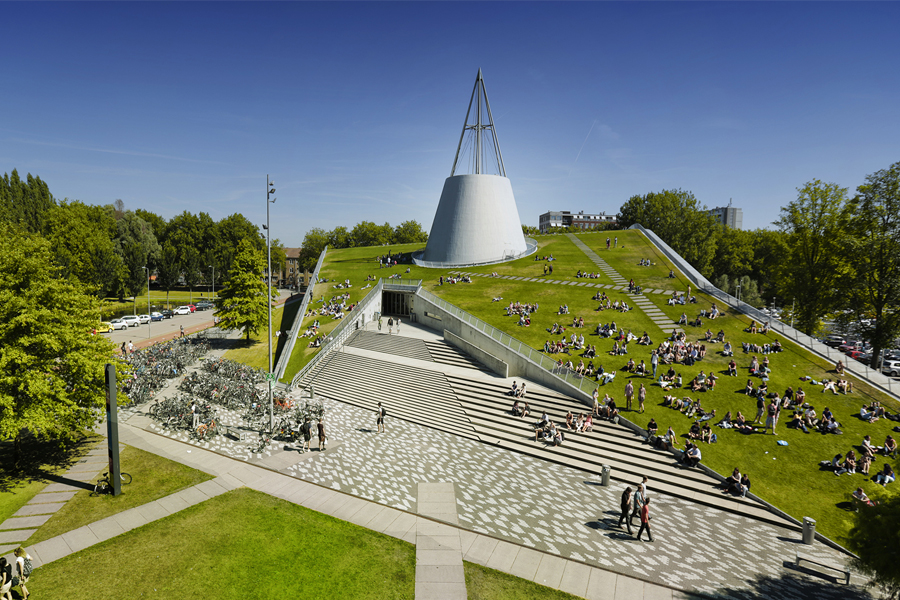
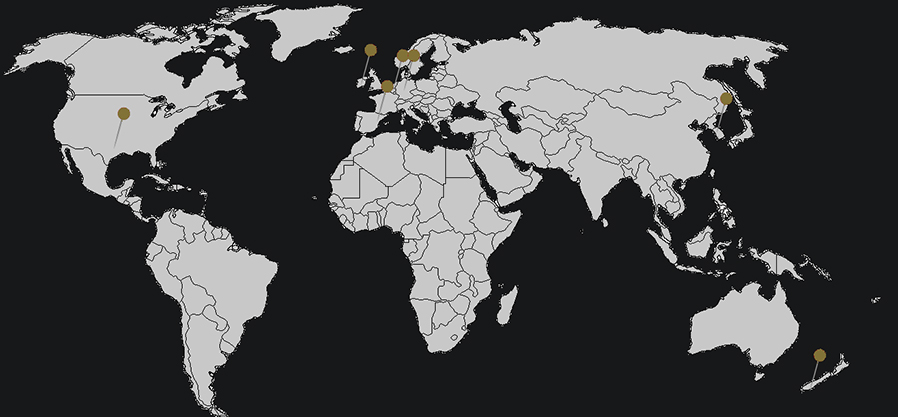
Collaborations
Our university partners in New Zealand, USA, Ireland, Korea, the Netherlands and Germany try to develop novel neuromodulation treatments for neurological and psychiatric disorders. This requires intense collaboration with technical universities, e.g., TU Delft in the Netherlands, and neuromodulation companies, such as Neuroelectrics, Soterix, and Abbott to develop novel neuromodulation technology, essential for the creation of new treatments.
On going projects
Neuromod Devices - TENT-A3 is a single arm repeated measures prospective investigation evaluating the safety and efficacy of the Lenire device for tinnitus treatment. The Lenire device provides non-invasive bimodal (sound and tongue) stimulation to alleviate the symptoms of chronic, subjective tinnitus. Participants presenting to one of the several study sites with a diagnosis of chronic subjective tinnitus who meet the inclusion criteria are enrolled in the investigation while the study site is active. The objective of TENT-A3 is to determine whether the addition of tongue stimulation to sound-only stimulation provides additional clinically significant improvements in tinnitus symptoms beyond that of the sound-only stimulation.
Horizon Europe - TARA project Chronic migraine is defined as a headache persistent for more than 3 months or a severe headache persistent for more than 15 days within a month. It affects approximately 2% of the world population. The World Health Organization classifies severe migraine attacks as among the most disabling illnesses, comparable to dementia and quadriplegia. Treatments start with pharmaceutical drugs, which have contra-indications and severe side effects and often remain ineffective in chronic migraine patients. Injectable treatments like Botox and nerve blocks can be effective but require multiple sessions per year and also have undesirable effects. Treatments using neurostimulation products that deliver electrical pulses to the occipital nerve have been up to 80% effective but they are designed for the back not the neck which results in high rates of surgical revisions. This leaves the chronic migraine population severely underserved and in need of an innovative solution and the TARA project partners aim to work together to services this gap. Our vision is fundamentally based on disrupting the continuum of care and referral pathway by creating a more effective non-surgical solution that reduces cost and risk and therefore increases accessibility to more physicians and patients. The consortium will develop a novel platform for the treatment of chronic migraine that will be particularly applicable to resource restricted environments and targeting underserved patients. We are working on 4 elements working together seamlessly: (1) A neurostimulation implantable device, (2) A wearable device that will power the implantable device, (3) A mobile app to control the implant, and (4) A delivery catheter that reduces tissue trauma and training required for physicians.
Tide consortium Research in clinical neuroscience is founded on the conviction that a better understanding of tinnitus related changes of brain function will improve our ability to diagnose and treat tinnitus. Although considerable advances have been made in understanding the mechanisms of tinnitus, the clinical management of tinnitus remains largely based on a ‘trial and error’ approach. The identification and validation of a biomarker for tinnitus is thought to be the crucial step in the development of a personalized approach to the diagnosis and treatment of tinnitus. The development of a biomarker in tinnitus would be ground-breaking and disruptive at the same time. It would advance patient management on a new level. By deriving two test paradigms from the most recent models of tinnitus, unpacking it in terms of depth of detail and breadth of application, and deploying it to explain wider aspects of the phenomenon than just the initial emergence of tinnitus, we seek for an objective marker for tinnitus or at least for a subtype of tinnitus related to a specific pathophysiology. This may have a major impact and fill the need of the pharmaceutical and hearing tech industry for biomarkers they require to start investing in tinnitus. In addition, this research has the potential to solve the still existing uncertainty about the pathophysiological mechanisms of tinnitus generation and maintenance. As our research aims to identify and validate a biomarker for the presence and intensity of tinnitus, the consortium has been designed to determine the phenotyping of a heterogeneous indication that will induce a paradigm shift in research, medicine, and society in how tinnitus is perceived and could lead to more awareness about the disease. Furthermore, it will markedly reduce one of the patients’ biggest frustrations, that they are not ‘taken seriously,’ that it is all in their mind, as the patients cannot prove they have tinnitus. The value of a biomarker could be enormous, including risk reduction associated with inappropriate treatment regimen or inability to detect an efficacy signal rapidly. Moreover, a valid biomarker will facilitate translational research.
NOE-TSS-201 study The goal to developing a treatment for debilitating disorders of the central nervous system, conditions charcterized by imbalanced neuronal networks leading to unresolved severe sympotoms and significant impact on patients` lives. This study is a double-blind, placebo-controlled, phaseII/III, multi-center prospectivre study to evaluate the efficacy and safety of Gemlapodect in Adult and Adolescent patients with Tourette syndrome.
Transcranial Near‑Infrared (tNIR) Light Therapy Low-power tNIR light-emitting diodes illuminate the light that is outside of the visible spectrum of human eyes but can efficiently penetrate the scalp, skull, and meninges to reach the brain parenchyma. It is proposed that mitochondrial dysfunction, inadequate supplies of adenosine triphosphate (ATP), and oxidative stress were contributory factors in burn-out and fatigue syndrome. This near-infrared photon absorption by cytochrome C oxidase might dissociate the inhibitory nitric oxide, unit IV of the mitochondrial respiratory chain, and thereby allowing the respiration to resume to be unhindered and to increase the ATP synthesis. The tNIR light could prove valuable for therapeutics by targeting the mitochondria, increasing ATP in proteasomes for ubiquitination of misfolded proteins, decreasing inflammation and even antibacterial and anti-viral effects leading to improvement in people suffering from a burn-out or fatigue syndrome.